Beginning on August 1, 2013, Florida began transitioning Medicaid recipients receiving or applying for long term care benefits into the new Florida Medicaid Managed Care Long Term Care Waiver, also known as Medicaid reform. The transition began with Region 7, which is the Orlando and Brevard County area. The transition will be implemented by region with the last regions coming on line on March 1, 2014.
During the transition, Florida’s Agency for Health Care Administration will notify Medicaid recipients of their Medicaid managed care plan choices and the deadline by which they must choose a plan. If a recipient fails or is unable to choose a managed care plan by the stated deadline, the state will automatically assign them to a plan. If a recipient is unsatisfied with the managed care plan they choose or have been automatically assigned to, they have 90 days during which they can change plans.
While the idea of a choice sounds easy, there are several steps a recipient must make in choosing a managed care plan. In making the choice, recipients must choose based on the type of institution in which they live or whether they live at home and whether they have applied for Medicaid or are a current Medicaid recipient. For an easy, step by step guide to making these choices visit Foundation for LTC Solutions. In addition, recipients must know who their health care providers are and whether those providers are a part of the the network the recipient chooses.
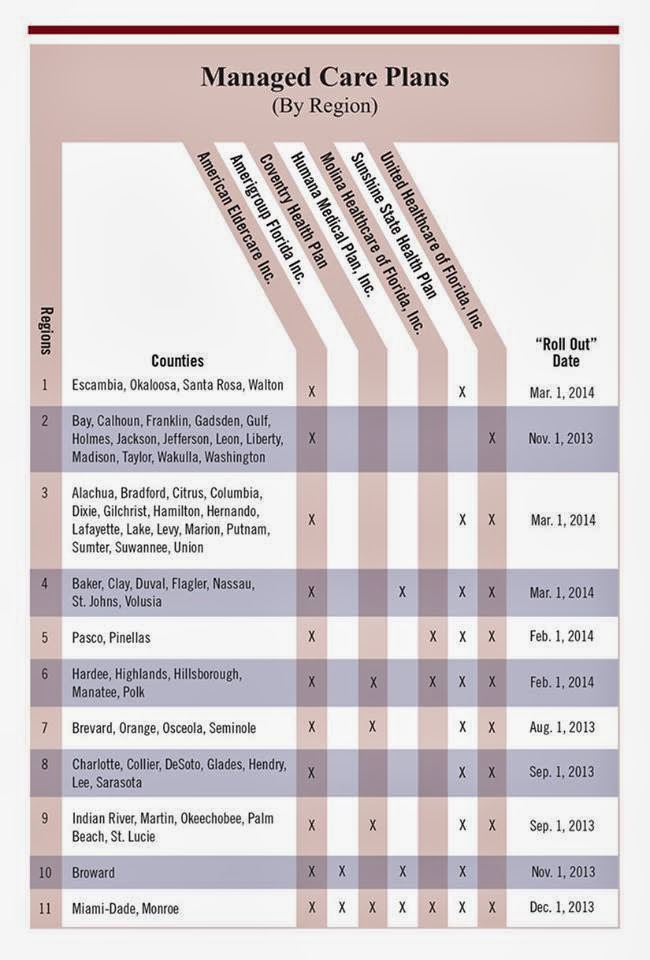
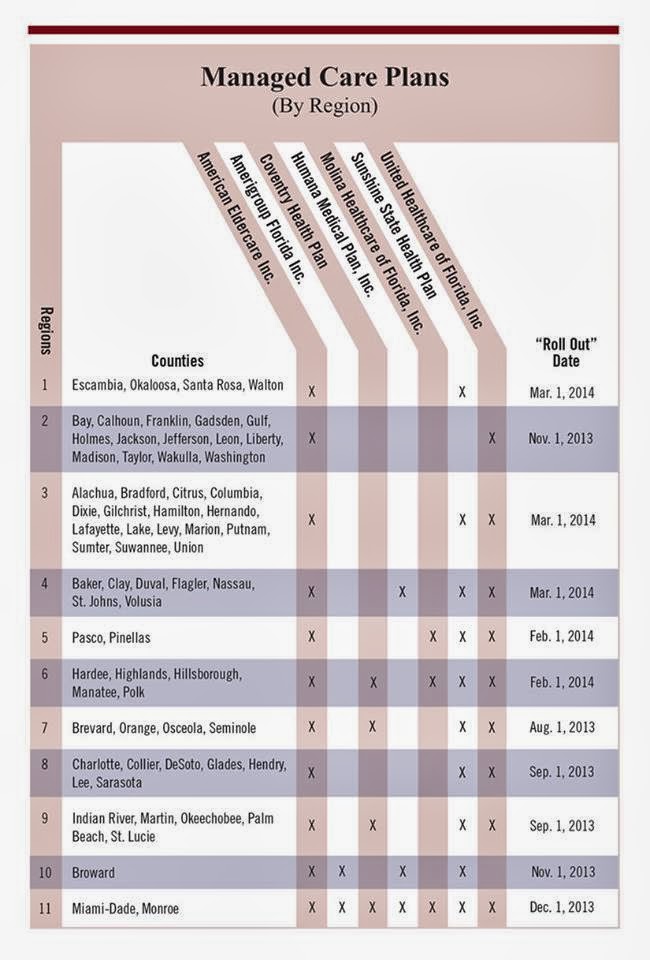
There are at least two managed care organizations in each Florida region with a total of seven plan. Only American Eldercare, Inc. provides services in each region. The following info graph provided by the Foundation for LTC Solutions shows all plans available in each region as well as the implementation date in each region:
If a recipient needs the assistance of a representative, surrogate, or agent to choose a managed care plan, there are additional steps that must be completed. The process by which someone is allowed to assist a recipient in making managed care plan choices is cumbersome and not consumer friendly. It can often lead to the state automatically enrolling the recipient in a managed care plan despite the consumer’s choice.
For information regarding the forms and process necessary to allow a representative, agent or health care surrogate to assist a recipient in making a managed care plan choice, visit Florida State Medicaid Managed Care Long Term Care Waiver. For problems faced by recipients using this system and possible solutions read Glitch Sessions on Foundation for LTC Solutions Facebook Page.
If you or someone you love is transitioning to the Florida Medicaid Managed Care Waiver program, feel free to comment on your experiences (good and bad) and provide any tips you may have found that make navigating this process easier.